
Injection technique: Top tips from a community nurse
Perhaps you have recently been prescribed insulin by your GP or diabetes nurse and you are feeling a little nervous about injecting yourself. Here is some advice to help you develop your confidence and technique.
By Jessica Trigg, Freelance Health Writer and Band 6 Registered Nurse, on best practice for injecting insulin for people living with diabetes.
Insulin kit checklist
Your GP or diabetes nurse specialist should have provided you with:
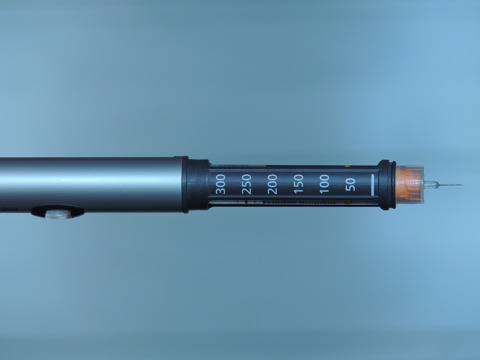
- An insulin pen. There are two main types of pens: pre-filled, which you can throw away after you have used it, or reusable with replaceable insulin cartridges. There are also smart insulin pens which are reusable pens that link to a person’s smartphone to help them record their doses, such as NovoPen 6, NovoPen Echo Plus and Tempo Pen.
- Sterile, single-use disposable needles, usually between 4mm-6mm in length.
- A blood glucose meter to check your blood glucose levels.
- Lancets and testing strips.
- Glucose in case you get an episode of hypoglycaemia (low blood glucose levels).
- Sharps container to dispose of needles and lancets, and a needle clipping device for when you are out and about.
You need to store any unopened insulin pens in the fridge, between 2-8°C.
Always keep at least one spare insulin cartridge/pen in the fridge and make sure it is not touching the cooling element at the back, or sitting too close to the freezer.
Once opened, your pen/cartridge can be used for 28 days before it expires. Remember to store your insulin in a dry, cool place, as too much sunlight or heat can damage it. It helps to write the date you opened your insulin on your pen to remind you when to discard it.

Technique
Insulin needs to be injected into the fatty layer of tissue beneath the skin. It should appear clear, not cloudy. Before injecting, make sure you have checked your blood glucose level. This should be above 4.0mmols/L. Check your prescription to see if you need to inject insulin before or with meals.
Steps to remember
- Wash your hands.
- Gently tip your pen up and down 20 times. Do not shake the pen as this causes bubbles which could affect the amount of insulin you inject. If you use soluble or long-acting insulin, skip this step.
- Attach a single-use needle and remove the inner and outer caps, holding the pen upright.
- Prime your pen: dial two units of insulin, and push the plunger down until a bead of insulin appears at the tip of the needle. This makes sure all the air is expelled before you inject into your skin.
- Choose your site: either your stomach, tops of your thighs or buttocks. It needs to be an area where there is some fatty tissue. Make sure the skin is clean and dry.
- Dial your dose: remember, insulin is prescribed in units, e.g. 20 units. Take care not to mistake the “U” of units for an “0” so that you do not overdose! If you are in any doubt, check the amount with your GP or diabetes nurse specialist.
- Use a 90-degree angle and push the needle all the way into your skin. If you don’t have much fat on your body, you can gently pinch your skin with two fingers with the opposite hand.
- Leave the needle under the skin for at least 5-10 seconds before withdrawing.
- Apply gentle pressure over the injection site for a few seconds after removing the needle.
Tips and troubleshooting
Here are a few common problems people experience:
Painful injections
Check your insulin is at room temperature. Cold insulin makes injections more painful, and the insulin takes longer to absorb.
If you are particularly sensitive to needles, try numbing the area with an ice cube for 15-20 seconds before you inject. If you have a longer needle, ask your GP/diabetes nurse if you can switch to a shorter one.
If you are still experiencing pain, consider an insulin injection aid, such as the TickleFLEX.
Redness, swelling or itching
It is normal for your skin to react to insulin, especially if this is the first time you are using it. If the area does not improve after several weeks or gets worse, contact your GP.
If you continue to experience skin irritation, you can discuss switching to a different insulin.
Remember to never reuse needles due to the risk of infection.
Bleeding and/or bruising
Some bleeding or bruising after injecting is to be expected from time to time. Apply gentle pressure for 5-10 seconds after injecting and avoid squeezing the skin too hard if you are using a pinch technique.
If you are bleeding regularly, speak to your GP to review your needle length to make sure you are not accidentally injecting into muscle. People using a longer needle can also try switching to a 45-degree angle when injecting.
Lumps and bumps
Sometimes lumps of fatty tissue gather under the skin due to injecting into the same place too often. The most common lumps are called lipohypertrophy (lipos). You can also develop a condition called cutaneous amyloidosis.
Lumps beneath the skin can interfere with insulin absorption and affect your blood glucose levels. It is important to alternate between the left and right side of your body each week and to make sure each new injection is at least one finger’s breadth away from the last site.
More information
Read NICE guidelines on Insulin therapy – type 2 diabetes
Read NHS patient information booklet on The safe use of insulin and you

About the author
Jessica Trigg is a freelance health writer and a registered nurse. Jessica has six years of experience working as a community nurse, caring for people living with long-term conditions.
Jessica currently works as a Clinical Research Nurse for Oxford University, alongside her clinical practice as a district nurse.
This article was originally published in the Autumn 2023 edition of Diabetes Wellness News. For more information and subscriptions click here
I would like to make a regular donation of
I would like to make a single donation of
There are lots of ways to raise money to support
people living with all forms of diabetes.
Bake, Swim, Cycle, Fly ... Do It For DRWF!
Fundraise with us
Recent News


